Executive Summary
After trauma scene cleanup in Columbus, the real work of healing begins. This article addresses the emotional recovery journey following traumatic loss, including understanding complex grief, navigating PTSD symptoms, accessing Columbus-area mental health resources, and developing sustainable coping strategies. Whether you’re days or months into recovery, this guide provides practical information about what to expect emotionally, when to seek professional help, and how to gradually rebuild your sense of safety and normalcy after tragedy has disrupted your life.
What Makes Healing After Trauma Scene Cleanup So Challenging?
Trauma scene cleanup addresses the physical aftermath, but emotional residue lingers long after surfaces are sanitized and belongings are restored. The challenge lies in the disconnect between external restoration and internal devastation.
Columbus families often describe feeling pressure to “move on” once the physical space is clean. Friends and extended family may assume that professional cleanup equals closure, not understanding that the real healing work is just beginning.
The brain processes trauma differently than ordinary grief. When you experience sudden, violent, or unexpected loss, your nervous system remains on high alert, constantly scanning for danger. This hypervigilance exhausts you mentally and physically, making normal functioning feel impossible.
Additionally, trauma disrupts your fundamental assumptions about safety, predictability, and control. When tragedy invades your home or involves someone you love, it shatters the illusion that following rules and being careful protects you from harm. Rebuilding these assumptions requires time and intentional effort.
What Psychological Conditions Commonly Follow Traumatic Loss?
Understanding potential mental health impacts helps you recognize when you need additional support.
Acute Stress Disorder: In the first month after trauma, many people experience intrusive memories, avoidance behaviors, negative mood changes, and heightened arousal. These symptoms are your brain’s normal response to abnormal circumstances.
Post-Traumatic Stress Disorder (PTSD): When acute stress symptoms persist beyond a month or worsen over time, PTSD may develop. This includes flashbacks, nightmares, severe anxiety, and uncontrollable thoughts about the event.
Complicated Grief: Unlike typical grief, complicated grief doesn’t soften over time. Intense yearning, preoccupation with the deceased, and inability to accept the death persist for more than a year.
Major Depressive Disorder: Trauma frequently triggers depression characterized by persistent sadness, loss of interest in activities, changes in sleep and appetite, and feelings of worthlessness or hopelessness.
Anxiety Disorders: Generalized anxiety, panic disorder, or specific phobias can emerge after trauma, creating persistent worry and physical symptoms like rapid heartbeat and shortness of breath.
These conditions are medical problems, not character flaws. They respond to treatment, and seeking help demonstrates strength and self-awareness.
A Story from Columbus: Michael’s Path Through Grief
Michael Torres lost his 19-year-old son, Jake, to an accidental overdose in their Columbus home in summer 2022. Michael, a construction supervisor and lifelong Ohio State fan, had always prided himself on being tough and self-reliant.
“Jake was home from college for the summer,” Michael recalls, his voice still thick with emotion. “I thought he was just sleeping in. When I went to wake him for our fishing trip, I knew immediately something was wrong.”
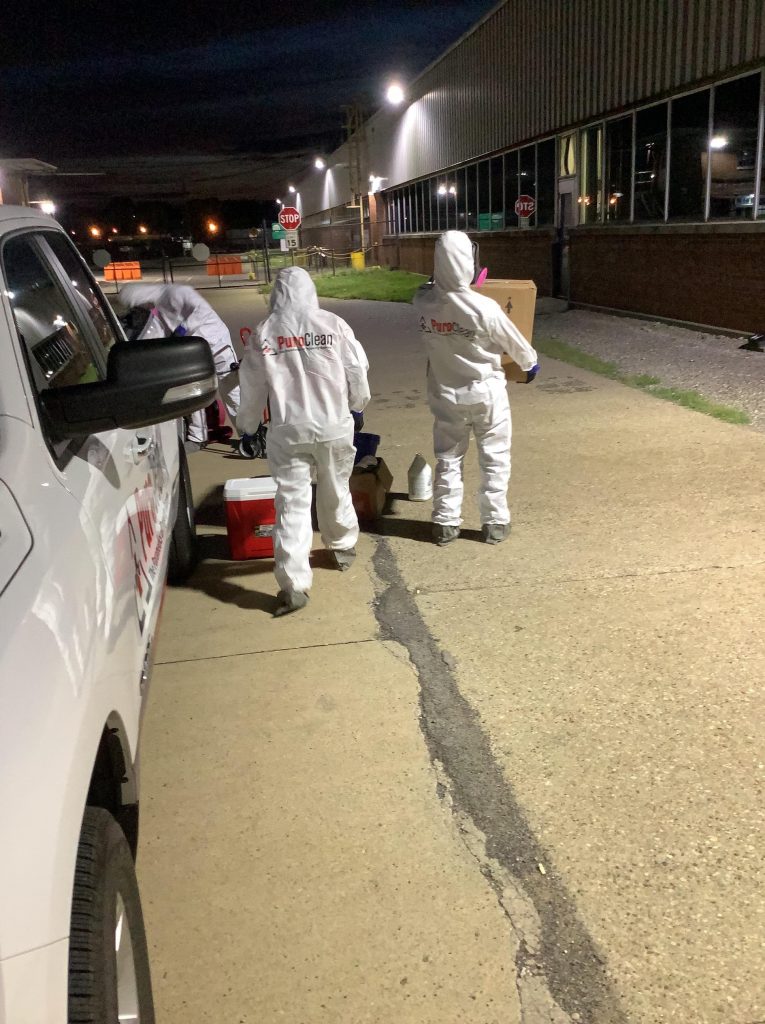
After emergency responders confirmed Jake’s death, Michael focused entirely on logistics. He called PuroClean Home Savers, arranged the funeral, notified relatives, and returned to work within a week.
“Everyone kept saying how strong I was being,” Michael says. “But I wasn’t strong. I was completely numb. I couldn’t feel anything.”
Three months later, the numbness cracked. Michael started having panic attacks at work. He couldn’t drive past the street where Jake had bought drugs. He stopped sleeping, haunted by questions about whether he’d missed warning signs.
“My wife finally made me go to the doctor. I thought I was having heart problems because my chest hurt constantly. The doctor said it was anxiety and gave me a referral to a therapist. I almost didn’t go. I kept thinking therapy was for weak people who couldn’t handle their problems.”
The turning point came during Michael’s first therapy session when his counselor explained how trauma affects the brain. “She showed me brain scans of people with PTSD. She explained that my brain was physically different because of what I’d experienced. It wasn’t about being weak or strong. My brain needed help healing from an injury.”
Michael began weekly therapy and joined a support group for parents who’d lost children to addiction at Nationwide Children’s Hospital. He learned breathing techniques for panic attacks and gradually exposed himself to triggers he’d been avoiding.
“The support group changed everything,” Michael reflects. “These were successful, educated, loving parents whose kids died anyway. It helped me understand that Jake’s death wasn’t my fault and that his addiction was stronger than my love.”
Two years later, Michael still attends monthly support group meetings and has become a peer mentor for newly grieving parents. He’s open about taking medication for anxiety and encourages other men to seek help without shame.
“Jake’s death will never make sense. But I can live with the loss now without it destroying me every single day. Some days are still terrible, but I’ve learned to ride those waves instead of drowning in them.”
What Are the First Steps Toward Emotional Recovery?
Beginning your healing journey requires small, manageable actions rather than dramatic transformations.
Acknowledge the reality: Denial serves a protective purpose initially, but healing requires gradually accepting what happened. This doesn’t mean you’re okay with it, just that you’re facing reality.
Prioritize physical needs: Grief and trauma suppress appetite, disrupt sleep, and drain energy. Even when you don’t feel like it, maintain basic nutrition, hydration, and rest. Your brain needs these fundamentals to heal.
Resist isolation: Trauma creates an urge to withdraw from others. While you need alone time, complete isolation intensifies symptoms. Stay connected with at least one or two safe people.
Limit major decisions: Avoid selling your home, changing jobs, or making other significant life changes for at least six months if possible. Trauma impairs judgment, and decisions made during acute grief often increase regret later.
Create structure: When internal chaos reigns, external structure provides stability. Maintain basic routines like showering, eating at regular times, and going to bed at consistent hours.
Practice self-compassion: You wouldn’t expect someone with a broken leg to run a marathon. Don’t expect yourself to function normally after emotional trauma. Give yourself the grace you’d extend to others.
Where Can Columbus Residents Access Mental Health Support?
Columbus offers extensive mental health resources specifically designed for trauma survivors.
OhioHealth Behavioral Health Services: Provides trauma-focused therapy, psychiatric services, and intensive outpatient programs throughout Columbus locations. They offer specialized trauma tracks that address PTSD, complicated grief, and co-occurring conditions.
Netcare Access: This 24/7 crisis hotline (614-276-2273) provides immediate telephone counseling, mobile crisis response, and connections to ongoing treatment. Use this service during acute crisis or when you’re unsure where to start.
Syntero (formerly Comcor): Offers affordable counseling services on a sliding scale based on income. They provide individual therapy, family counseling, and support groups.
The Ohio State University Wexner Medical Center: Their psychiatric department specializes in trauma treatment, including EMDR therapy, CPT, and medication management.
Maryhaven: Specifically addresses addiction-related trauma and loss, offering specialized grief support for families affected by overdose deaths.
Columbus Area Suicide Survivors: Provides peer support groups specifically for people who’ve lost loved ones to suicide, meeting monthly at various Columbus locations.
NAMI Columbus: The National Alliance on Mental Illness offers free education programs, support groups, and resource navigation for individuals and families dealing with mental health conditions following trauma.
How Do You Know When You Need Professional Mental Health Treatment?
Some people heal with support from friends and family, while others require professional intervention. These signs indicate you should seek professional help.
Symptoms that worsen over time: If anxiety, depression, or intrusive thoughts intensify rather than gradually improving after the first month, professional treatment can prevent further deterioration.
Interference with daily functioning: When trauma symptoms prevent you from working, maintaining relationships, or caring for yourself or dependents, you need additional support.
Substance use changes: Increasing alcohol consumption, using drugs to cope, or developing concerning patterns with prescription medications signals the need for intervention.
Suicidal thoughts: Any thoughts about ending your life require immediate professional attention. Call 988 (Suicide and Crisis Lifeline) or go to the nearest emergency room.
Physical symptoms without medical cause: When doctors rule out physical illness but symptoms persist, trauma may be manifesting somatically through your body.
Relationship deterioration: If trauma is destroying your relationships with partners, children, or other important people, couples or family therapy can help.
Anniversary intensification: If symptoms dramatically worsen around anniversaries or specific triggers, therapy can help process these reactions.
What Evidence-Based Therapies Work Best for Trauma Recovery?
Not all therapy is created equal for trauma treatment. These specific approaches have strong research support.
EMDR (Eye Movement Desensitization and Reprocessing): This therapy helps reprocess traumatic memories using bilateral stimulation (eye movements, tapping, or sounds). Many people experience significant relief within 8-12 sessions.
Cognitive Processing Therapy (CPT): Specifically designed for PTSD, CPT helps you examine and challenge thoughts about the trauma that keep you stuck in unhealthy patterns.
Prolonged Exposure Therapy: This approach gradually exposes you to trauma-related memories, feelings, and situations you’ve been avoiding, reducing their power over time.
Trauma-Focused Cognitive Behavioral Therapy: Combines cognitive restructuring with gradual exposure, helping you develop more adaptive thoughts and behaviors.
Grief Therapy: Specialized grief counseling addresses the unique challenges of sudden, traumatic, or complicated loss.
Group Therapy: Sharing your experience with others who’ve faced similar traumas reduces isolation and provides practical coping strategies from peers.
When seeking a therapist, ask specifically about their training and experience with trauma. General counselors may lack the specialized skills needed for trauma recovery.
What Role Does Medication Play in Trauma Recovery?
Medication isn’t necessary for everyone, but it can provide crucial support during acute phases of recovery.
Antidepressants (SSRIs): Medications like sertraline (Zoloft) or paroxetine (Paxil) are FDA-approved for PTSD and can reduce anxiety, depression, and intrusive thoughts.
Anti-anxiety medications: Short-term use of medications like lorazepam can help during acute crisis, though long-term use risks dependence.
Sleep aids: Addressing sleep disturbances is crucial for healing. Medications like trazodone or prazosin (which reduces nightmares) can restore restorative sleep.
Mood stabilizers: For some people, medications that stabilize mood swings support emotional regulation during recovery.
Medication works best when combined with therapy rather than as a standalone treatment. Discuss options with a psychiatrist who specializes in trauma rather than relying solely on primary care prescribing.
How Do You Rebuild a Sense of Safety After Trauma?
Trauma shatters your sense of security. Rebuilding it requires deliberate effort.
Establish safety routines: Actions like checking locks, installing security systems, or having someone stay with you initially aren’t paranoid; they’re your nervous system’s need for tangible safety measures.
Create a calming environment: Modify your space to promote relaxation. This might include softer lighting, comfortable textures, calming colors, or meaningful objects that provide comfort.
Practice grounding techniques: When anxiety spikes, grounding exercises reconnect you with the present moment. Try the 5-4-3-2-1 technique: identify 5 things you see, 4 you can touch, 3 you hear, 2 you smell, and 1 you taste.
Develop a safety plan: Write down steps to take during panic attacks or when suicidal thoughts emerge. Include crisis numbers, supportive people to contact, and self-soothing activities that have worked before.
Reclaim your space gradually: If trauma occurred in your home, you don’t need to immediately occupy that space. Gradually approach it with support, making small changes to create visual and emotional distance from the event.
What Coping Strategies Support Long-Term Healing?
Beyond professional treatment, these practices support sustained recovery.
Mindfulness and meditation: Even five minutes daily of focused breathing or guided meditation can regulate your nervous system and reduce anxiety over time.
Physical movement: Exercise releases endorphins, reduces stress hormones, and provides a healthy outlet for tension. Start small with walking or gentle yoga if intensive exercise feels overwhelming.
Creative expression: Art, music, writing, or other creative outlets help process emotions that words alone cannot capture.
Nature exposure: Time outdoors, especially in green spaces, measurably reduces stress and improves mood. Columbus Metro Parks offer easily accessible natural spaces.
Meaningful connection: Quality time with safe people who understand your grief provides essential emotional support.
Spiritual practices: For those who find comfort in faith, prayer, religious community, or spiritual contemplation can provide meaning and hope.
Helping others: When you’re ready, volunteering or supporting others who’ve faced similar losses can transform pain into purpose.
How Should You Handle Difficult Conversations About Your Loss?
Talking about trauma is challenging, especially when others don’t understand or say hurtful things unintentionally.
Set boundaries: You’re not obligated to discuss details with everyone. “I appreciate your concern, but I’m not ready to talk about it” is a complete sentence.
Prepare responses: Having standard responses to common questions (“How did it happen?” or “Are you doing better?”) reduces the emotional tax of repeated explanations.
Educate when appropriate: Some people genuinely want to understand and support you but don’t know how. Brief education about trauma or grief can help them offer better support.
Protect yourself from toxic positivity: Well-meaning people often offer platitudes like “Everything happens for a reason” or “They’re in a better place.” These minimize your pain. You can politely decline to engage: “I know you mean well, but that doesn’t help me right now.”
Find people who get it: Support groups connect you with people who truly understand because they’ve lived through similar experiences.
What If You’re Caring for Children While Processing Your Own Trauma?
Parenting through trauma presents unique challenges that require balancing your healing with your children’s needs.
Be honest age-appropriately: Children sense when something is wrong. Honest explanations appropriate to their developmental level build trust and reduce anxiety.
Maintain routines: Children need predictability even more during crisis. Keeping schedules consistent provides security when everything feels uncertain.
Allow their unique grief expressions: Children grieve differently than adults. Respect their process even when it doesn’t match yours.
Get them professional support: Child therapists specializing in trauma use play therapy, art therapy, and other age-appropriate techniques to help children process loss.
Take breaks when needed: You can’t pour from an empty cup. Having trusted adults temporarily care for your children while you attend therapy or rest isn’t abandonment; it’s necessary self-care that ultimately makes you a better parent.
Model healthy coping: Children learn emotional regulation by watching adults. When you practice healthy coping strategies, you teach them valuable skills.
When Should You Return to Work After Traumatic Loss?
There’s no standard timeline for returning to work. Consider these factors when deciding.
Financial necessity: If you must return quickly for financial reasons, communicate with your employer about needed accommodations like flexible hours or working from home initially.
Workplace support: Employers vary dramatically in their support for grieving employees. Assess whether your workplace offers employee assistance programs, bereavement leave beyond the standard few days, or flexibility during your recovery.
Your readiness: Some people find work provides helpful structure and distraction. Others can’t focus and need more time. Both responses are valid.
Type of work: Jobs requiring high concentration, emotional labor, or public interaction may be more challenging during acute grief than routine physical work.
Phased return: Many people benefit from gradually increasing hours rather than immediately returning full-time.
How Do You Navigate Social Situations When You’re Still Grieving?
Social events can feel overwhelming when you’re navigating trauma recovery.
Give yourself permission to decline: You don’t owe anyone your presence at social gatherings. Protecting your energy is more important than meeting others’ expectations.
Leave when you need to: If you attend an event and become overwhelmed, leaving early isn’t rude. People who care about you will understand.
Bring support: Having someone with you who understands your grief can provide security and an exit strategy if needed.
Prepare responses: Plan brief answers to questions about how you’re doing so you’re not caught off-guard.
Engage selectively: You don’t need to participate fully in every aspect of gatherings. It’s fine to sit quietly or step outside when you need space.
What If Your Relationship Is Struggling Under the Weight of Grief?
Couples often struggle after traumatic loss because partners grieve differently.
Understand different grieving styles: One partner might need to talk constantly while the other processes internally. Neither approach is wrong.
Schedule connection time: Grief can cause couples to become roommates rather than partners. Intentionally spending quality time together maintains your bond.
Attend couples counseling: A therapist can help you communicate about differing needs, navigate conflicts related to grief, and maintain intimacy during this challenging time.
Resist blame: Trauma sometimes creates a need to assign responsibility. Blaming your partner for things outside their control damages your relationship without changing what happened.
Maintain physical intimacy: Grief often reduces sexual desire, but maintaining physical connection through touch, cuddling, or hand-holding sustains emotional intimacy.
Frequently Asked Questions
How long should I expect to feel this way?
Acute grief symptoms typically peak in the first 6-12 months and gradually soften over 2-3 years. However, trauma adds complexity that can extend this timeline. PTSD symptoms may not appear until months after the event. Everyone’s timeline is unique and influenced by support systems, previous trauma, relationship to the deceased, and whether you engage in treatment.
Is it normal to feel angry at the person who died?
Yes, anger at the deceased is extremely common and completely normal. This is especially true with deaths by suicide or overdose, where it feels like the person chose to leave you. Anger is a natural grief stage and doesn’t mean you didn’t love them or aren’t sad about their death.
What if I can’t afford therapy?
Columbus offers many affordable options. Syntero provides sliding-scale counseling based on income. NAMI Columbus offers free support groups. Some churches provide free pastoral counseling. Online therapy platforms like BetterHelp often cost less than traditional therapy. Many therapists reserve a few sliding-scale spots in their practice.
Should I sell my home if the trauma happened there?
Don’t make this decision during the first six months if possible. Many people initially feel they must sell but later find they can reclaim the space with time and therapy. Others genuinely cannot heal in that environment. Give yourself time to make this significant decision with a clearer mind.
How do I support my partner when we’re both grieving?
Communicate about different needs and respect that you may grieve differently. Attend couples counseling to navigate this together. Create space for individual processing while maintaining connection. Remember you’re on the same team even when grief drives you apart temporarily.
What if people at work don’t understand why I’m still struggling?
Unfortunately, many workplaces lack understanding about grief timelines. You might share educational resources about complicated grief or PTSD with supervisors. Request specific accommodations through HR. Focus on communicating your needs rather than convincing others you’re suffering enough.
When will I stop having nightmares and flashbacks?
These intrusive symptoms are hallmarks of PTSD and typically don’t resolve without treatment. EMDR therapy, CPT, or prolonged exposure therapy specifically address flashbacks and nightmares. Medication like prazosin can reduce nightmare frequency while you’re doing therapeutic work.
Is it okay to feel moments of happiness or normalcy?
Absolutely yes. Feeling joy, laughing, or having normal moments doesn’t dishonor your loved one or mean you’re healing too fast. Grief comes in waves; between waves, moments of peace or happiness are healthy and necessary.
Conclusion
Healing after trauma scene cleanup in Columbus is a journey without shortcuts. The physical restoration that professionals provide in hours represents just the beginning of emotional recovery that unfolds over months and years. This healing isn’t linear; you’ll have good days and setbacks, progress and regression, hope and despair.
What matters is that you don’t face this journey alone. Columbus offers extensive resources staffed by professionals who understand trauma’s impact and can guide you toward recovery. Seeking help isn’t weakness; it’s the brave recognition that trauma is bigger than any individual and requires support to overcome.
Your loved one’s death changed you permanently. Healing doesn’t mean returning to who you were before; that person no longer exists. Instead, healing means integrating this loss into your identity, learning to carry the grief while still engaging with life, and eventually finding meaning and purpose even after profound loss.
If you’re in Columbus or surrounding communities dealing with the aftermath of a traumatic scene, PuroClean Home Savers provides compassionate, professional cleanup services that restore your physical space with dignity and respect. Their team understands the emotional weight of what you’re experiencing and handles every situation with the sensitivity it deserves. For immediate assistance, call PuroClean Home Savers at (614) 689-0012. They’re available 24/7 to help you take the first step toward reclaiming your space and beginning your healing journey.


